Microbiome study could change the way doctors diagnose depression
"To keep gut health is to keep mental health."
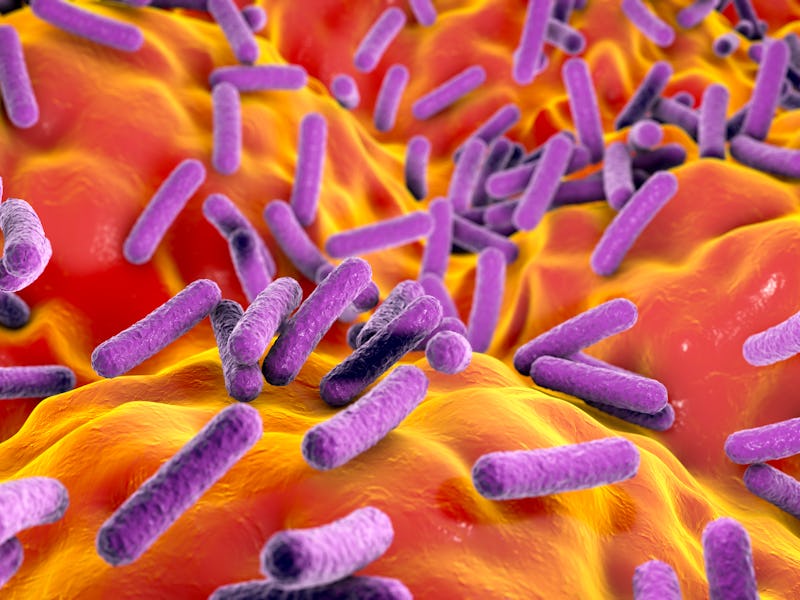
In our body, deep within the gut, live trillions of bacteria, fungi, protozoa, and viruses. Collectively, this diverse community is known as microbiota. The human microbiome is the aggregate of this internal ecosystem.
The microbiome influences everything from immune function to the digestive system. New research adds further proof that it may also profoundly affect the brain.
By analyzing the fecal samples of 311 people, scientists discovered evidence linking gut microbiome disturbances to major depressive disorder. The findings highlight fascinating links between gut health and mental health — and charts a path toward a potential tool capable of diagnosing and treating depression.
"The disturbed gut ecosystem, characterized by the microbiome, virome, and fecal metabolomics, is closely linked to our mental well-being," study co-author Shaohua Hu tells Inverse. Hu is a psychiatrist at the First Affiliated Hospital at the Zhejiang University School of Medicine in China.
"To keep gut health is to keep mental health."
The study was published Wednesday in the journal Science Advances.
Gut check — Psychologists or psychiatrists typically rely on interviews to diagnose individuals with major depressive disorder, also known as clinical depression. They ask about mental health symptoms like feelings of hopelessness, lack of motivation, anger outbursts, or trouble with sleep. Unfortunately, these clinical interviews can frequently result in misdiagnosis. In primary care practices, misdiagnoses outnumber missed cases of depression.
As a potential solution to this problem, scientists are eager to pinpoint biomarkers of depression — measurable indicators of a state or condition, like proteins in the brain, that could give patients a better shot at an accurate diagnosis. However, the underlying molecular basis of depression remains "mostly obscure," Hu and his team write in the new study.
To make clear this ambiguity, this team honed in on the gut microbiome. They recruited 311 people — 155 healthy participants and 156 participants with major depressive disorder. They collected the study subject's fecal samples, which offer a glimpse at the gut ecosystem.
The team, in turn, identified distinct bacterial compositions in patients with depression compared to healthy participants. They pinpointed three bacteriophages, 47 bacterial species, and 50 fecal metabolites that were significantly different in people with major depressive disorder compared with healthy people.
Those with depression contained higher levels of bacterial species belonging to the genus Bacteroides, which they say could be linked to higher cytokine levels and increased inflammation. They also observed lower levels of species belonging to Blautia and Eubacterium compared to the healthy controls, which could result in a loss of anti-inflammatory benefits.
What's next? — Based on these differences, researchers developed a biomarker panel that they hope can one day offer a companion to clinical interviews. The tool could eventually offer extra information for diagnosing clinical depression, and be developed as a "treatment target, Hu says.
"In daily practice, clinicians should pay special attention to the gastrointestinal discomfort in patients with mental disorders, such as constipation, diarrhea, and other functional abnormalities," Hu says. These could be a "mirror" of the dysregulated microbiota-gut-brain axis.
Supplements, like probiotics or prebiotics, could also be utilized as a "clinical choice to alleviate depressive symptoms in some individuals," Hu says.
It's still too early to say that definitive mental health diagnoses can be made based on the gut microbiome. But researchers are increasingly paying attention to this "gut-brain axis," hypothesizing that the gut bacterial microbiome plays a role in Parkinson's disease, bipolar disorder, and autism.
However, at this stage, questions dwarf answers. The dynamic between gut health and mental health is complex and bidirectional. It's likely that gut microbiome disturbances negatively influence mental health. Simultaneously, changes in diet and physical activity associated with mental health problems may, in turn, harm the gut microbiome.
The genetic makeup of clinically depressed individuals, the depression itself, and altered lifestyles due to depressive episodes can all have significant influences on the gut microbiome, Hu says.
Further research exploring the gut-brain axis will elucidate this complicated relationship.
For now, to keep the gut healthy and functioning optimally, experts suggest: eating lots of fibrous, nutrient-rich vegetables and yogurt, drinking kombucha, and exercising regularly. In specific situations, such as replenishing gut bacteria after recovering from an infection or pathogen, your doctor may suggest adding a pre-or probiotic to your routine.
"In daily life, people should be careful about their diet pattern, exercise, and medications that are known to have effects on gut microbial diversity and compositions," Hu explains. "Gastrointestinal discomfort may be a physical sign of mental illnesses."
Abstract: Gut microbiome disturbances have been implicated in major depressive disorder (MDD). However, little is known about how the gut virome, microbiome, and fecal metabolome change, and how they interact in MDD. Here, using whole-genome shotgun metagenomic and untargeted metabolic methods, we identified 3 bacteriophages, 47 bacterial species, and 50 fecal metabolites showing notable differences in abundance between MDD patients and healthy controls (HCs). Patients with MDD were mainly characterized by increased abundance of the genus Bacteroides and decreased abundance of the genera Blautia and Eubacterium. These multilevel omics alter- ations generated a characteristic MDD coexpression network. Disturbed microbial genes and fecal metabolites were consistently mapped to amino acid (g-aminobutyrate, phenylalanine, and tryptophan) metabolism. Furthermore, we identified a combinatorial marker panel that robustly discriminated MDD from HC individuals in both the dis- covery and validation sets. Our findings provide a deep insight into understanding of the roles of disturbed gut ecosystem in MDD.