This elusive toxin in the gut reawakens "zombie" viruses
Colibactin has been confounding scientists for almost two decades. New research uncovers one piece of the puzzle.
An elusive molecule lurking in the human gut may have the ability to awaken “zombie” or latent viruses hiding in the microbiome, new research shows.
A team of researchers, led by chemical biologist and Harvard Medical School professor, Emily Balskus, uncovered the stealth mechanisms by which colibactin, an important but cryptic molecule generated by some microbes in the gut, wreaks havoc on cells. Their results, published last week in Nature, represent a significant leap in understanding colibactin’s ability to activate dormant viruses in the gut. A better understanding of how this works could help researchers better treat conditions that wreak havoc on the gut.
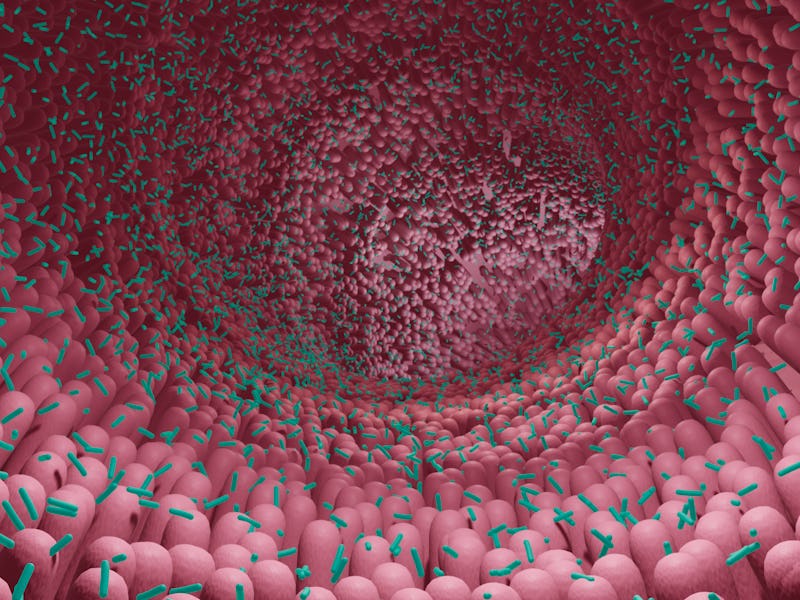
Our bowels are home to countless microorganisms including bacteria, viruses, and fungi. Not all of these microbes are harmful; many are either harmless or beneficial to our health. Researchers also know that bacteria themselves can also be home to viruses. These typically remain dormant unless activated or “awakened.”
“It’s known that changes to the human gut and virome are associated with human disease, including things like Inflammatory Bowel Disease,” Balskus tells Inverse. “What is less known [is] what influences the activation of these latent viruses in the gut. That’s the question we sought to answer in this study.”
What you need to know first— Scientists have long known that colibactin can gravely damage human cells, but the precise mechanism by which this damage occurs was unknown. The consequences of such damage are better understood; previous research has shown an association between the molecule and colorectal cancer. Research suggests that colibactin derived from E. coli induces DNA double-strand breaks and interstrand DNA cross-links, which can cause cancer. Specifically, colibactin is associated with as much as 67 percent of colon cancers.
In 2006, researchers in France found that the DNA of mammalian cells was fatally damaged after encountering the gut bacteria E.coli. The researchers determined the resulting damage was due to a cluster of E.coli genes. E. coli is a very common bacteria found in the gut microbiome and is typically innocuous. However, researchers found certain strains of E. coli contain genetic blueprints for producing a byproduct, a toxic molecule. The molecule was dubbed colibactin.
Styimiying research, however, was how difficult it proved to isolate colibactin from the bacteria from which it emerged.
How the discovery was made— Balskus’s lab has long studied colibactin— their research is among the evidence connecting colibactin to colorectal cancer. Yet they too struggled to isolate the molecule from the bacteria that produced it.
The gut microbiome is a diverse colony of bacteria. Colibactin is one toxic byproduct of specific strains of bacteria.
A breakthrough in the colibactin mystery came when two researchers in Balskus’s lab questioned how colibactin, given how unstable it is, could remain alive long enough to enter bacterial cells. They hypothesized that another factor could be at play; specifically, a bacteria-infecting virus.
The researchers tested the hypothesis by growing colibactin-producing bacteria alongside a different kind of bacteria: one that carries latent viruses. The researchers hoped this ex-vivo recreation of one part of the microbiome would allow them to document how colibactin operates in the microbiome.
What they found— While the researchers found that colibactin could indeed enter cells and damage DNA, their experiments confirmed a major part of their hypothesis: the DNA damage from the colibactin triggered something catastrophic; when the colibactin producers came into contact with bacteria containing latent viruses, the number of viral particles increased and the growth of virus-containing bacteria dropped. This viral boom resulted in a surge of “active, cell-killing infections,” the researchers report.
Somehow, colibactin is able to tweak microbial cells in such a way that latent viruses come back to life and, like The Walking Dead, outcompete its non-zombified counterparts.
“We hypothesize that this bacteria probably evolved to target other bacteria,” Balskus tells Inverse. “So if we can gain a better understanding of why colibactin is being made, we may be able to formulate some strategies to stop bacteria from making it.”
Digging into the details— Not every cell is susceptible to colibactin’s damage. Many microbes are able to protect themselves from the harmful effects of colibactin. Balskus and her colleagues identified a resistance gene encoding a protein that neutralizes colibactin in a variety of bacteria.
Balskus doubts that causing disease is colibactin’s sole function. What would make sense is much more basic evolutionary biology: this virus awakening lethal activity may simply be how colibactin outcompetes other bacteria in the very crowded microbiome.
What it means for the future— While Balskus’s team has made a huge leap in understanding how colibactin causes cellular damage, there’s still a lot that remains unknown.
“We’d like to really try to now investigate the consequence of kind of awakening these latent viruses,” Balskus says. “We don’t have a great understanding of the precise triggers for these types of events. And so now that we’ve identified one factor, we can hopefully do some work in animal models to try to figure out what happens to the viral component of the gut microbiome, and what consequences might that have for the host.”
Uncovering how colibactin does some of its damage may or may not help us fight colon cancer. But given colibactin’s clear association with cancer, finding any missing piece of the puzzle is cause for celebration.
This article was originally published on