A new understanding of lung cells could lead to better Covid-19 treatment
"There are mechanisms that are in-built evolutionarily that means these macrophages are resistant to infection."
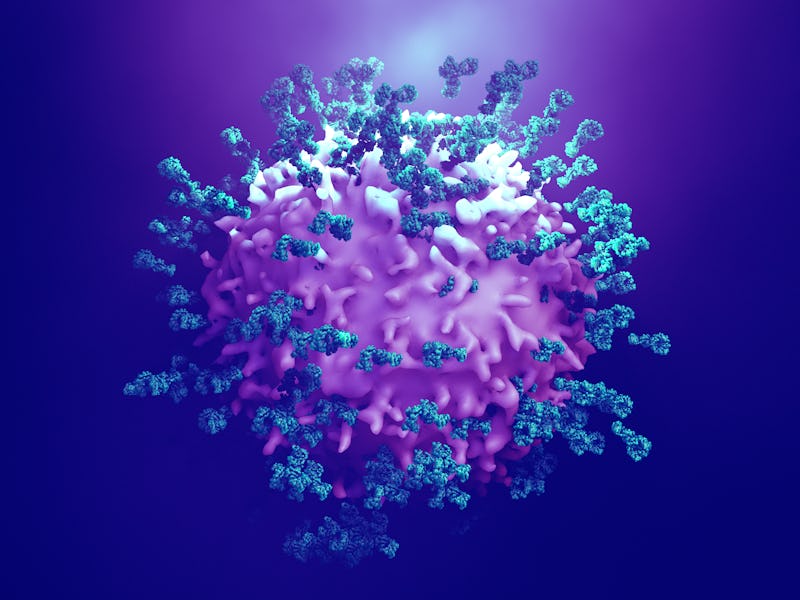
The science on the novel coronavirus and what it does to the body is preliminary and evolving every day. But one thing is known for sure: that Covid-19 wreaks the worst of its havoc in the lungs.
In a new study, published Friday in the journal Science Immunology, scientists shed some light on how, exactly, our respiratory organs fight back against the virus.
Until now, scientists believed there was only one major population of a type of white blood cell known as macrophages in the lungs, called alveolar macrophages.
But the new research highlights the role of another macrophage also found in the lungs, called nerve- and airway-associated macrophages, or NAMs. These cells appear to cluster near the airways and the pulmonary nerves of the lungs – hence their name.
These cells are similar to the better known and well-studied alveolar macrophages, but they are distinct in their shape, and, it seems, their function.
Instead of clearing out pathogens like alveolar macrophages do, these cells appear to control inflammation and suppress the immune response.
In the event of an infection, like Covid-19, the body fights back aggressively — this means that the infection can be taken down quickly, but it can also cause excessive inflammation and damage to the cells. NAMs appear to keep this damage under control.
Coronavirus control
To discover how these cells react to an infection, the researchers infected mice with the flu virus. They then conducted live-cell imaging and genetic analysis on the mice to try and understand the cells' function.
Face-to-face with a viral infection, “these macrophages had this uncanny ability to increase in number,” study senior author Kamal Khanna, an associate professor of immunology at NYU Langone Medical School, tells Inverse.
“They proliferated quite a bit.”
The genetic analysis reveals these cells have immunosuppressant capabilities, meaning they diminish the wrath of the body's immune response to an infection.
Next, the researchers created transgenic mice models lacking the NAMs. As a result, these mice experienced massive amounts of inflammation upon infection.
Interestingly, when they carried out the imaging studies with the alveolar macrophages, they saw they were instantly infected with influenza. But the NAMs were found to be completely resistant to infection.
“That is really fascinating,” Khanna says, “because that tells us that there are mechanisms that are in-built evolutionarily that means these macrophages are resistant to infection.”
The cells are also present in humans' lungs. Encouragingly, Khanna and his team found that they appear to be largely the same in shape and function as those seen in the mice.
The findings may be important for the understanding of other respiratory infections and diseases — including Covid-19, Khanna says. This study did not examine the relationship between these macrophages and the novel coronavirus.
Owing to the increasing gravity of the situation with Covid-19, however, Khanna says, "the million-dollar question now is: what do these macrophages do in human beings?”
Treatment timeline
Khanna and his team are now going to look at the function of these cells in older people. It is possible that, in older individuals, these macrophages are not working as well.
On the other hand, it is also possible that these macrophages are working too well, and have taken over the lungs, causing “a very immunosuppressive environment — too much of an immunosuppressive environment,” Kamal says.
To treat a viral infection effectively requires a delicate balancing act, Khanna says.
"You get the immune system revving up early and you bring down the viral load. But, at the same time, that immune system revving up can be very damaging to the tissue, and you need to bring that down.”
That matters when it comes to medical interventions, Khanna explains.
“If you intervene with immunosuppression too early, you'll cause damage," he says.
"If you intervene with immunosuppression at the perfect time, when the viral load is low enough and can be cleared, but immunopathology is increasing, that's where you help the patient."
These new findings illuminate the ways in which the lungs work to control excessive inflammation in the face of infection. The study is in mice, so the results are preliminary and will need to be further researched in humans to know how far they apply to humans. But Khanna says he feels the pressure to get these results out there, at this crucial time, to help to inform treatments.
“What I would like to do is just to contribute to the clinical side of things. People can then figure out what would work best," he says.
Abstract: Tissue-resident macrophages are a diverse population of cells that perform specialized functions including sus- taining tissue homeostasis and tissue surveillance. Here, we report an interstitial subset of CD169+ lung-resident macrophages that are transcriptionally and developmentally distinct from alveolar macrophages (AMs). They are primarily localized around the airways and are found in close proximity to the sympathetic nerves in the broncho- vascular bundle. These nerve- and airway-associated macrophages (NAMs) are tissue resident, yolk sac derived, self-renewing, and do not require CCR2+ monocytes for development or maintenance. Unlike AMs, the develop- ment of NAMs requires CSF1 but not GM-CSF. Bulk population and single-cell transcriptome analysis indicated that NAMs are distinct from other lung-resident macrophage subsets and highly express immunoregulatory genes under steady-state and inflammatory conditions. NAMs proliferated robustly after influenza infection and activation with the TLR3 ligand poly(I:C), and in their absence, the inflammatory response was augmented, result- ing in excessive production of inflammatory cytokines and innate immune cell infiltration. Overall, our study pro- vides insights into a distinct subset of airway-associated pulmonary macrophages that function to maintain immune and tissue homeostasis.