Cord blood helped cure a woman of HIV. Can it treat other diseases, too?
The new approach raises hopes for helping more people.
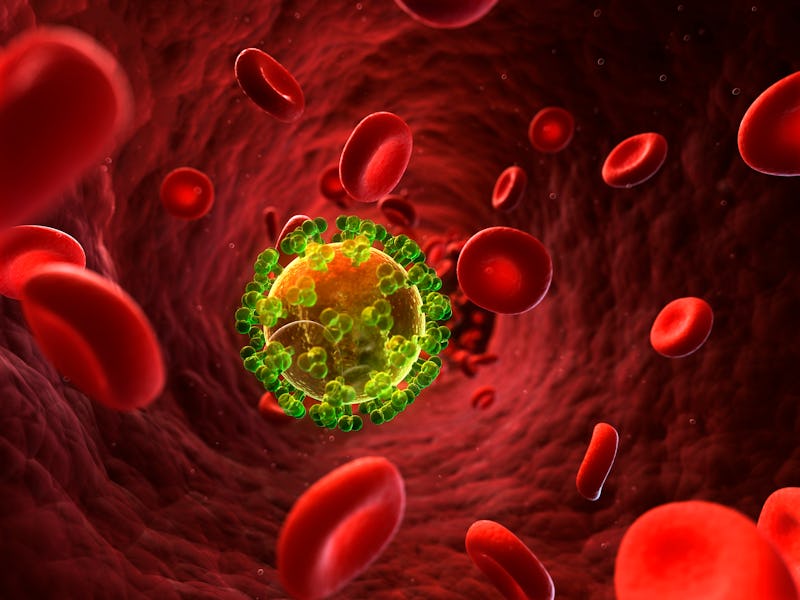
A woman in the U.S. has become the third person to possibly be cured of HIV through medical treatments, scientists reported last week.
Back in 2017, the woman (who was described as middle-aged) was treated for leukemia using transplanted umbilical cord blood. More than four years later, her cancer remains in remission — and the researchers can’t find any trace of HIV in her body.
That’s particularly significant because the woman is of mixed race, unlike the two men previously cured of HIV using bone marrow transplants. The milestone raises hopes that the new approach could cure some HIV patients who are only partial genetic matches with their donors.
“This opens up additional options for people to find a match,” Yvonne Bryson, the chief of pediatric infectious diseases at the David Geffen School of Medicine at UCLA, who presented the findings on February 15 at the Conference on Retroviruses and Opportunistic Infections in Denver, tells Inverse. “It’s especially another option that’s relevant…for more diverse populations.”
There’s a big caveat here: Bone marrow and cord blood transplants are too dangerous to be a good choice for most people with HIV. The procedures are typically given to people with cancer and certain other diseases to replace damaged cells; physicians wipe out the patient’s immune system and then infuse healthy, blood-forming stem cells that are free of cancer.
“You have to get rid of your own cells by massive chemo and radiation therapy,” Paul Goepfert, an HIV expert and director of the Alabama Vaccine Research Clinic at the University of Alabama at Birmingham, who wasn’t involved with the research, tells Inverse. “It's nothing you would do unless you have some other really serious underlying condition for which you need a bone marrow transplant.”
Such was the case for Timothy Ray Brown and Adam Castillejo, both of whom were diagnosed with blood cancers after living with HIV for years. The men received the transplants from donors with a rare mutation that happened to make their cells resistant to HIV infection. However, this mutation is mostly found in people of northern European ancestry. Bryson and her collaborators knew that bone marrow from donors with this mutation would be unlikely to help their patient.
“Cord blood is more forgiving,” she says. “It doesn’t require that close a match.”
Another advantage of cord blood is that it’s more readily available than bone marrow. But there are some challenges, too. Cord blood contains fewer stem cells and they grow more slowly, leaving recipients vulnerable to infections. To protect their patient until the mutated cord blood cells took over, Bryson’s team also gave her blood stem cells from a relative.
“She had an HIV-resistant immune system after the cord blood populated, and she still has that 100 percent-resistant immune system even now,” says Bryson, who presented the findings on February 15 at the Conference on Retroviruses and Opportunistic Infections in Denver.
Even after the patient stopped taking antiretroviral therapy, the researchers could not detect HIV in her cells. When they exposed samples of the woman’s cells to several HIV strains in the laboratory, the virus was unable to take root.
She also endured fewer side effects than Brown and Castillejo did after their bone marrow transplants. The spry young cord blood cells may be the reason the woman didn’t develop graft vs. host disease, which occurs when the donated stem cells attack the body. These “newborns” might be more adaptable, Koen Van Besien, director of the transplant service at Weill Cornell Medicine, where the patient was treated, told the New York Times. The strategy of supplementing cord blood with a relative’s stem cells might benefit around 50 patients with HIV and cancer per year in the US, he told NBC News.
Because of its limited number of stem cells, cord blood is more often used to treat children than adults. Bryson sees the technique her team developed as an opportunity to make the transplants accessible to more adult cancer patients with and without HIV. “We need to push for considering cord bloods as an untapped source and also provide some mechanisms for screening these cord bloods on a routine basis” for the beneficial mutation, she says.
The handful of cases in which people have sent HIV into remission with stem cell treatments—or spontaneously cleared the infection—suggest “that there’s something we can figure out that can cure people with HIV,” says Goepfert. “So there are lots of avenues and I think people are very excited.”
If some of these methods pan out, he says, they could also be applied to other chronic viral infections like hepatitis B. Some promising approaches include genetically engineering cells to make them resistant to HIV or attack infected cells, using lab-made antibodies to block infection, locking the virus in a dormant state, and “shock and kill” strategies to target the “reservoir” of HIV lurking in the DNA of infected immune cells.
“For finding an HIV cure, it seems there's more than just one thing that needs to be done: one, reducing the virus to undetectable [levels] and reducing the reservoirs as well, and secondly to create an immune system that will block it from rebounding,” Bryson says.