Is The Gut Microbiome Actually Our “Friend”? One Scientist Says No
While we might think we derive health benefits from our uninvited houseguests, the theory of evolutionary addiction begs otherwise.
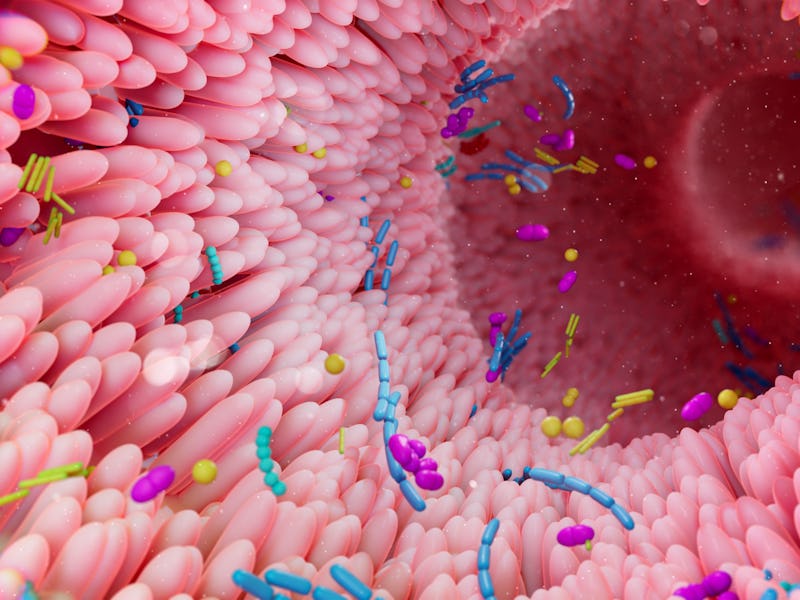
The story of the microbiome is often portrayed as blissful mutualism: Throughout human evolution, the trillions of microbes colonizing every square inch of our bodies found ways to make their uninvited stay beneficial for us. Numerous studies suggest that the microbiome plays a key role in keeping us healthy while it’s in balance and putting us at risk for disease when it’s not. The microbiome has been implicated in everything from longevity to weight loss to Alzheimer’s disease and mental health.
But scientists like Tobin Hammer, assistant professor of ecology and evolutionary biology at the University of California, Irvine, are more skeptical of this buddy-buddy situation. In an opinion article published last fall in the journal Trends in Microbiology, Hammer posits that we’re in a kind of Stockholm syndrome with microbes conscripting themselves into essential physiological functions simply because they’re around, not because they are enhancing or improving our well-being. He calls this phenomenon “evolutionary addiction.”
Inverse spoke with Hammer about how our “friends with benefits” relationship with the microbiome may be anything but.
The interview below has been edited and condensed for clarity.
The popular perception of the microbiome is that it confers numerous health benefits. In your paper, you argue that our relationship with the microbiome is more of an “evolutionary addiction.” What is that?
This is when a dependency arises without a benefit. In the paper, I give the example of caffeine addiction from my own personal experience. If I don’t have caffeine, I do really badly. You could argue that caffeine benefits me because when you remove it, I malfunction, essentially. But most people wouldn’t consider a substance you’re addicted to, to be beneficial for fundamental parts of your behavior and physiology.
Analogous to that, a host may be able to do something on its own, and then as it evolves with its microbiome, those microbes can become necessary to perform a certain function. Going back to the coffee analogy, before I started drinking coffee, I could go about my day perfectly fine. If you compare myself before starting to drink coffee to now, there actually hasn’t been any real benefit or improvement. But when you remove it, then I can’t do all these basic things.
But wouldn’t that still suggest that the microbiome is vital for health or well-being in some capacity?
In any specific example, it’s hard to rule out the possibility that microbes are providing some important and unique service. It’s well known that in humans, gut bacteria digest food and produce short-chain fatty acids, and those feed into a lot of aspects of physiology. I’m not questioning those mechanisms and benefits because microbes are doing something unique that we can’t do.
The real issue is: Have the microbes improved our ability to perform these essential functions? In some cases, they have, and in some cases, I would argue they haven’t. The tricky thing is that the data can look the same with both processes, whether removing the microbiome [or not].
What are the different ways that can bring about evolutionary addiction?
One mechanism is called adaptive accommodation. Basically, it’s the early stages of a host interacting with a microbiome or a whole microbiome. The host is adapting itself to the presence of microbes, kind of incorporating their presence into how it regulates its physiological processes.
In some cases, these microbes might start as parasites, and so the host is evolving to better defend or tolerate the presence of the parasite. In doing so, they become dependent on it. For example, the layer of mucus lining the colon. It’s been known for many decades that if you remove or disrupt the gut microbiome, there’s a much thinner layer of mucus lining the gut, and that can lead to all sorts of problems, especially pathogens crossing and infecting the gut lining. The benefits-centric explanation is that microbes are helping us regulate the mucus layer — they promote gut homeostasis. But it’s easy to think how this might have arisen via adaptive accommodation because a lot of gut bacteria eat mucus. If you want to maintain your mucus layer, it makes sense to make more mucus when you sense that there are these new disturbing bacteria. You’re incorporating microbial cues into gut function.
Another mechanism is compensated trait loss. This starts with a microbe compensating for a function you can already do. There are lots of examples of this: Your [body] might perform some enzymatic reaction, and a microbe that’s become part of your microbiome can also do it. Because you have this redundancy, if you stop performing this function, it doesn’t matter because the microbe is compensating. The functionality doesn’t change, but now there’s a dependency. If you remove the microbe, the function completely stops because the host’s [innate] ability has degenerated.
Is there a significant overlap between our own innate physiological functions and those that microbes may compensate for?
It’s hard to think of it in terms of what percentage [of overlapping] function but there are a lot of biochemical reactions that are deeply conserved. You will find related enzymes in both bacteria and animals. It’s not necessarily that microbes are producing the exact same metabolites. There’s a paper that argues microbes provide a lot of molecules that can be used for signals, and the host incorporates those into how they regulate processes like development or immunity. They’re not necessarily better signals, but they work just fine.
Are there any other potential mechanisms driving evolutionary addiction?
There’s an interesting one known for decades [but] no direct evidence for it — it’s more of a proof-of-concept where you have a toxin-antitoxin dependency.
Basically, it comes from plasmids, which are extra-chromosomal DNA molecules that can force their host cell to maintain them. These plasmids encode toxin-antitoxin systems where they make both a toxin and antidote. The trick is that the toxin persists longer than the antidote. So imagine: a plasmid is cranking out both toxin and antidote. As long as both of them are in the cell, there’s no toxicity. But if you remove the plasmid, you have toxin persisting longer, outliving the antidote. You could call it an addiction of the host cells to these genetic elements.
How would we be able to test evolutionary addiction?
I want to acknowledge that it’s going to be very difficult, if not impossible, to test [this theory] in most systems. I think that for a lot of systems ... we can kind of guess whether a certain dependency is missing benefits [when a certain trait is missing because a microbe is missing] or evolutionary addiction.
Where I think there’s going to be the most potential are laboratory hosts that we can raise, have short generations of, and do experimental evolution. We can then see [if] these addictions are rising as hosts are adapting or evolving in the presence of microbes.
The microbiome may be more of a covert foe than a selfless friend. Where does this theory of evolutionary addiction fit into the field of probiotics, especially considering there’s much debate over whether such supplements are effective?
One consideration is that in evolutionary addiction, the evolution part is important. The hosts are evolving these dependencies; either they’re adapting through adaptive accommodation or compensated trait loss, but that, of course, takes time. Benefits [from probiotics] are a potentially immediate effect. If there is some magical probiotic you could take that would immediately benefit you that doesn’t require any evolution to occur, I don’t think there are going to be any short-term effects or new dependencies. I don’t think it’s a factor or a concern for probiotics.
I think the biggest impact is a little more philosophical, coming back to this idea of “Is the microbiome our friend?” I also think a core part of this is whether we should be surprised to see these microbial effects on all these different host processes. In the literature, there’s certainly a very large element of surprise, and I’m not saying it’s not amazing. I’m arguing that you can view the microbiome as another feature of the environment. If you suddenly change the organism’s environment, a lot of things are going to go wrong. No one should be surprised by that.