New "Person on a Chip" Technology Means Miniature Hearts and Livers
Thumbnail-sized models of human organs are making animal and human drug testing obsolete.
Is the human body really that complicated? Researchers from the University of Toronto have succeeded in distilling parts of the human body onto a piece of software not much bigger than a stamp. Nicknamed “person-on-a-chip” technology, the tiny chips, housing millions of living human cells, act as substitutes for real organs in drug testing and could make expensive and high-risk animal and human models obsolete. While the idea isn’t new — organs on chips have been created before — the officially-named AngioChips are remarkable not only for their ability to model actual organs but also the interactions between them.
In a paper released this week in the journal Nature Materials, a Canadian team of researchers describe how tiny scaffolds, made up of 3D-printed layers of a biodegradable and biocompatible polymer known as POMaC, provide the architecture for miniature versions of real-life hearts and livers.
Each chip, about the size of a thumbnail, is perforated with microscopic channels that, once the whole thing is submerged in a bath of living cells, act as the mini-organ’s internal blood vessels. In time, the heart or liver cells latch onto the structure and grow — and eventually behave — in the same way they would in the human body.
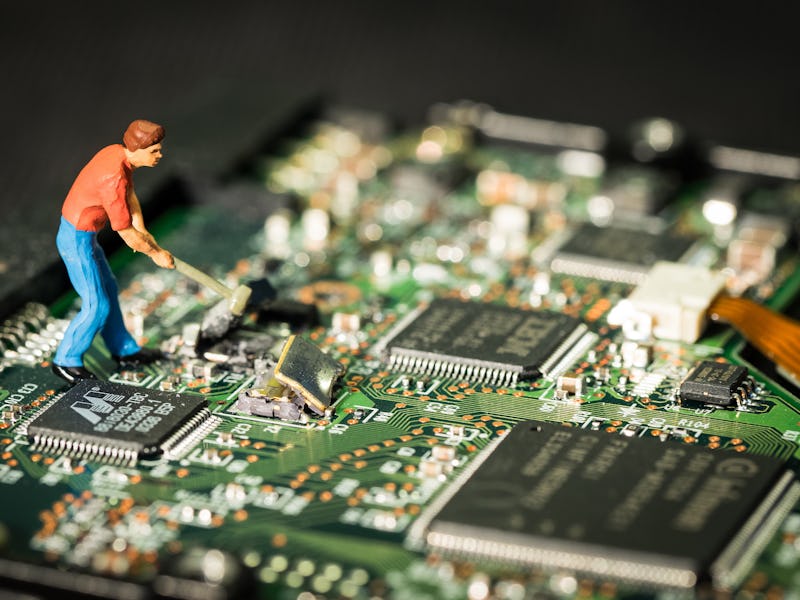
An example of the chip scaffolding.
Injected with clinically relevant drugs through their network of blood vessels, the AngioChips were shown to process drugs in the same way organs would in the actual human body. Like puzzle pieces, the AngioChips and their vessels can also be attached to each other, effectively creating a tiny model of an interlinked lung and heart.
To prove how seamlessly the chips function as miniature organs, the researchers went ahead and implanted one into a rat’s hind leg, documenting how the rat’s blood seamlessly squeezed through the 3D-printed blood vessels, seemingly naturally. Such functions will be especially useful, the researchers report, for linking together cells from, say, a cancerous tumor and the human heart, and seeing whether a drug could destroy one and not the other.
Commercializing the AngioChips hasn’t happened yet — lead author Milica Radisic, Ph.D. is working on it through her spin-off company TARA Biosystems Inc. — but this isn’t likely to be a problem for the researchers, considering this new technology just skyrocketed the researchers to the forefront of the mini-organ game. But let’s be real — some extra funding would be a much-needed boost for the researchers, considering that each of the tiny multi-layered scaffolds are painstakingly put together by hand.