A Novel Anti-Aging Treatment Revitalized Mice Immune Systems — Will It Work In Humans?
One group of researchers believe they’ve found a way to reset the immune system with a one-time antibody treatment.
You might know your immune system as the built-in, around-the-clock surveillance system primed to keep nasty germs out and swiftly kick to the curb any that do manage to sneak in. It’s a system primed to protect us at any age, but the sad truth is that once we get older, our immunity slows down and wanes.
But what if there was a way to get back that pep in our immune step? Amidst a rising wave of anti-aging research seeking the keys to rejuvenation, one group of scientists led by Stanford University and the National Institutes of Health believe they’ve found a way to reset the immune system with a one-time antibody treatment.
These findings were published Wednesday in the journal Nature.
Myeloid versus lymphoid
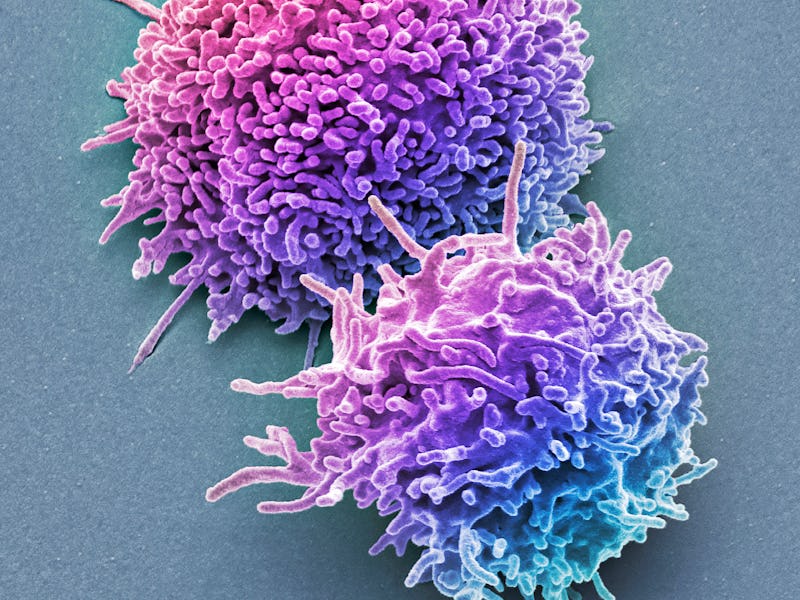
The treatment relies on rebalancing a group of cells called hematopoietic stem cells (HSCs) that live in our bone marrow. These HSCs are the progenitors of other blood and immune system cells, and as we age, they tend to give rise to more blood, or myeloid, cells rather than lymphoid or immune cells like B and T cells. The researchers found that when older mice were given an antibody treatment targeting myeloid-making HSCs, this resulted in a stronger immune system that responded faster to vaccination and was less prone to unnecessary inflammation.
“Older people just don’t make many new B and T cell lymphocytes,” Irving Weissman, the study’s lead researcher and professor of pathology and developmental biology at Stanford University, said in a press release. “During the start of the COVID-19 pandemic, it quickly became clear that older people were dying in larger numbers than younger people. This trend continued even after vaccinations became available. If we can revitalize the aging human immune system like we did in mice, it could be lifesaving when the next global pathogen arises.”
Lymphoid cells like B and T cells (also known collectively as lymphocytes) make up the adaptive immune system, which is more specific and strategic, and keeps a record of past tussles. Some myeloid cells also have immune functions, but they’re part of another division called innate immunity. This system is non-specific and triggers responses like inflammation to help with protection and recruit other immune cells to the fold. While inflammation in and of itself isn’t bad, it tends to stir up more and without due cause as we age, coining a phenomenon scientists have dubbed “inflammaging.”
Why some HSCs tend to make more myeloid cells — skewing the balance between myeloid and lymphoid cells — isn’t entirely understood. But there’s evidence to suggest that extremely long-lived people don’t experience this skew and, as a result, retain protective B and T cells that help them mount fast and effective immune responses and likely less inflammation.
Rebalancing the immune force
In the new study, Weissman and his colleagues explored whether it was possible to realign HSCs with an antibody therapy. Because antibodies are very specific in who or what they target, the researchers need to make sure they go after HSCs bending towards myeloid and not lymphoid cells. They examined the surfaces of mouse HSCs and found three proteins that singled out potential pro-myeloid versus lymphoid cells.
Antibodies designed to seek out and destroy these myeloid-biased HSCs were injected into older mice, about 18 to 24 months of age (roughly equivalent to 56 to 69 years old in human years). The numbers of myeloid and lymphoid cells were measured one week, eight weeks, and 16 weeks later. Their numbers were compared against younger mice aged three to six months old, or about 20 to 30 years old in human years. One group of older mice didn’t receive the treatment.
After one week, the antibody-treated older mice demonstrated a considerable decrease in the number of pro-myeloid HSCs, and this effect seemed pretty durable, lasting up to 16 weeks compared to their untreated counterparts. The treatment didn’t harm HSCs inclined toward lymphoid cells; there were a lot more new B and T cells circulating in animals’ bodies.
“Not only did we see a shift toward cells involved in adaptive immunity, but we also observed a dampening in the levels of inflammatory proteins in the treated animals,” Jason Ross, the paper’s first author and a postdoctoral medical fellow at Stanford University, said in the press release. “We were surprised that a single course of treatment had such a long-lasting effect. The difference between the treated and untreated animals remained dramatic even two months later.”
The researchers also saw that when the antibody-treated older mice were vaccinated eight weeks later against a virus to which they had never been exposed before, their immune systems responded swiftly, not exactly on par with the younger mice but following close.
Concerns for future research
As with many studies involving animals, they set a precedent of potentially reaping the same benefits in humans, but running in parallel, the caution that our mileage may widely vary.
Writing in a commentary accompanying the study, stem cell biologist Robert Signer and Yasar Arfat Kasu of the University of California, San Diego, said the research offers a tantalizing new direction in rejuvenating aged immune systems. Yet there are still unknowns and concerns, in particular, whether or not this novel antibody treatment could affect clonal hematopoiesis, an age-related phenomenon where a group of HSCs carry the same genetic mutation and start to multiply and potentially outnumber and overpower all other HSCs.
“[The authors of the new paper] contend that targeted depletion of myeloid-biased HSCs could preferentially eradicate these dominant or pre-cancerous HSC clones. However, antibody conditioning could, in fact, exacerbate the emergence of clonal hematopoiesis by narrowing the total repertoire of HSCs,” write Signer and Arfat Kasu. This, in turn, they add, may instead accelerate one’s “progression to cancer.”
Weissman and Ross are hopeful, however, that what they have demonstrated in mice will work and be beneficial to humans since they found that the pattern of genes switched on in aged mice with myeloid-biased HSCs is similar to the ones found in humans.
“This is a real paradigm shift — researchers and clinicians should think in a new way about the immune system and aging,” said Ross. “The idea that it’s possible to tune the entire immune system of millions of cells simply by affecting the function of such a rare population is surprising and exciting.”