An Antibiotic-Resistant Stomach Bug is on the Rise — Should You Be Worried?
The CDC issued a warning about increased cases of antibiotic-resistant Shigella, which adds to the growing antibiotic resistance crisis.
If you’ve come down with the stomach flu recently, chances are you’re not alone. Outbreaks of norovirus — a pathogen that often causes severe vomiting and diarrhea — are surging in the U.S., Canada, and the U.K in recent weeks. In the U.K., health officials say reported cases are 66 percent higher than what’s typically seen in the country at this time of year.
Norovirus is more of a nuisance than a public health crisis — after a couple of miserable days, the GI bug tends to clear up on its own. But experts worry we might be in for a long stretch since the virus is so hard to get rid of. To add insult to injury, we’re also seeing a rise in antibiotic-resistant Shigella, a bacteria that, in a similar manner, spread from person-to-person, causing severe diarrhea and intestinal infection called shigellosis.
Last Friday, the CDC released a health advisory warning that cases of antibiotic-resistant Shigella have risen by five percent in 2022 from virtually zero percent in 2015. Historically, Shigella tends to be most severe in children and the elderly, but the agency has also reported a rise in cases among other groups, such as people experiencing homelessness, international travelers, men who have sex with men, and people with HIV.
This comes at the heels of many other worrisome viruses and bacteria, aside from Covid-19, we’ve seen in recent years — monkeypox, respiratory syncytial virus, and invasive strep A infections, to name a few. Adding another pathogen to the mix makes the Last of Us feel closer to an apocalyptic reality. How worried should we actually be?
What is Shigella?
Shigella is a family of rod-shaped bacteria that likely descended millions of years ago from a mutated Escherichia coli, a gut-residing bacteria that’s generally harmless but has a few pathogenic strains that can cause severe illness, Robert Frenck, director of the Vaccine Research Center at Cincinnati Children’s Hospital, tells Inverse.
Compared to other bacteria like tuberculosis or viruses like the flu or monkeypox that usually have an animal “middleman” before jumping to humans, Shigella is exclusively a human-based pathogen. This means the bacteria is primarily spread through an infected person, whether via personal contact, fecal-oral route (so poop), or through contaminated food and water.
Shigella is a rod-shaped bacteria much like E. coli and Yersinia pestis, which caused the Plague.
Unlike other bacteria that cause diarrhea and gastrointestinal illness, you don’t need to come in contact with a lot of Shigella to get sick, which makes it easy to spread to others.
“It takes probably somewhere around 1,000 Shigella [organisms] to make you sick,” says Frenck. “That’s one microgram — one-millionth of a gram — of stool to infect you… That’s why it’s really easy to pass from person to person within a household.”
What are the symptoms of shigellosis?
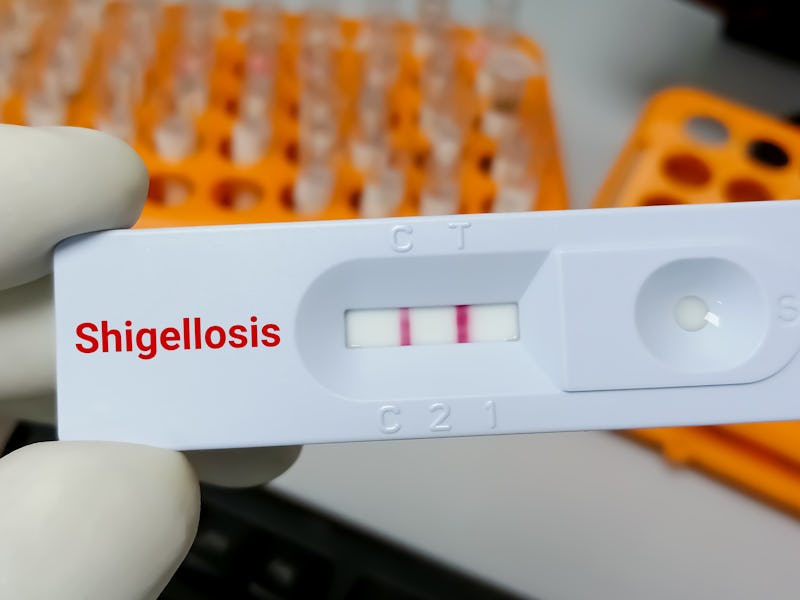
Once you’re infected with the bacteria, the incubation period — the time it takes for an infection to develop once you’ve been exposed — is 12 to 96 hours. Diagnosis is made with a stool test, and the main symptoms are really bad diarrhea, abdominal pain and cramps, a loss of appetite, and fever, William Schaffner, professor of preventive medicine and infectious diseases at Vanderbilt University School of Medicine, tells Inverse.
“[The] biggest hazard in the very young and the very old and frail is dehydration because of diarrhea,” he says.
There are two antibiotics, ciprofloxacin and azithromycin (or Zithromax), that are recommended for treating shigellosis (the medical term for a Shigella infection), and that’s where an antibiotic-resistant Shigella complicates things, increasing the time it takes for some folks, particularly those vulnerable to severe infection, to clear the microbe. But the good news, says Frenck and Schaffner, is that antibiotic-resistant or not, shigellosis is self-limiting as long as you get adequate rest and hydration.
“As long as you keep up with your fluid, you will recover,” says Schaffner. “Of course, it will take you longer to recover [if you get antibiotic-resistant Shigella], and you will be infectious to others for a longer period of time, a matter of days up to a week.”
Mild to moderate dehydration is common in patients with shigellosis.
Because shigellosis is a huge burden in developing countries where access to clean water is scarce, researchers like Frenck are working on a vaccine that helps the body develop immunity against the bacteria. While it will take several years before we have a Shigella-targeted jab on the market, Frenck says it most likely will be deployed in areas hardest hit by shigellosis and for international travelers who are at risk for getting the bacteria.
Rise of antibiotic resistance
So if Shigella is a bit of a bacterial nothing burger, what’s the concern? Simply, antibiotic resistance.
In the last several years, bacteria growing resistant to all sorts of antibiotics is becoming a threat to global health. In 2019, deaths due to antibiotic-resistant infections tolled at 1.27 million — more deaths than HIV/AIDS or malaria — 32,000 of those deaths were in the U.S. alone.
The rise of this antibiotic-resistant Shigella adds fuel to the antimicrobial resistance fire, says Frenck and Schaffner, because the pathogen can pass along drug-resistance genes to other bacteria within the gut.
“The genetic element that causes the multiple drug resistance is what’s called a mobile piece of DNA [also known as a plasmid],” says Schaffner. “As these Shigella get in touch, for example, with E. coli that are in our guts, [they] can get close to each other [and] this genetic element could be potentially transmitted to the E. coli or other similar bacteria that are co-resident in the intestines.”
Our takeaway: Practice good hygiene!
Frenck and Schaffner say the key to preventing Shigella transmission comes down to this: Practicing good hygiene.
“The biggest thing with all diarrheal diseases, the best protection is hand washing,” says Frenck, as well as practicing safe sex practices like wearing a condom.
Soap and water remove certain germs that hand sanitizers don’t kill such as diarrheal bacteria and norovirus.
To prevent antibiotic resistance overall, Schaffner says there’s been a move within the healthcare community to be more prudent and careful in using and prescribing antibiotics, the misuse and overuse of which have been associated with accelerating the antibiotic resistance crisis. According to the CDC, the agency has scheduled a call on February 28 to brief clinicians about the increase in drug-resistant Shigella infections and how to manage it.
This article was originally published on