China's Latest Antibiotic Resistance Crisis Proves Honesty Defeats Plagues
Super-resistant bacteria evolve not just because antibiotics are used irresponsibly, but because no one admits it.
The discovery of penicillin in the 1920s ushered in the antibiotic era and ushered out the age of bacterial massacres. For roughly a century now, humanity has enjoyed protection from most infectious diseases while bacteria have continued along their evolutionary path, being selected for their fitness in a drug-enhanced world. Now, many are resistant to antibiotics and it feels like only a matter of time until the plagues return. But, as Timothy Walsh, Ph.D., an infection and immunity expert at Cardiff University, points out, that amount of time matters considerably. Walsh claims that honesty about how we use antibiotics can extend their usefulness — hopefully long enough for scientists to find an alternative.
“We definitely need to have a much greater sense of accountability in terms of antibiotic resistance,” Walsh told Inverse. Super-resistant bacteria evolve when antibiotics are overprescribed or used incorrectly, but Walsh says avoiding this is difficult because people lie and lying has become profitable.
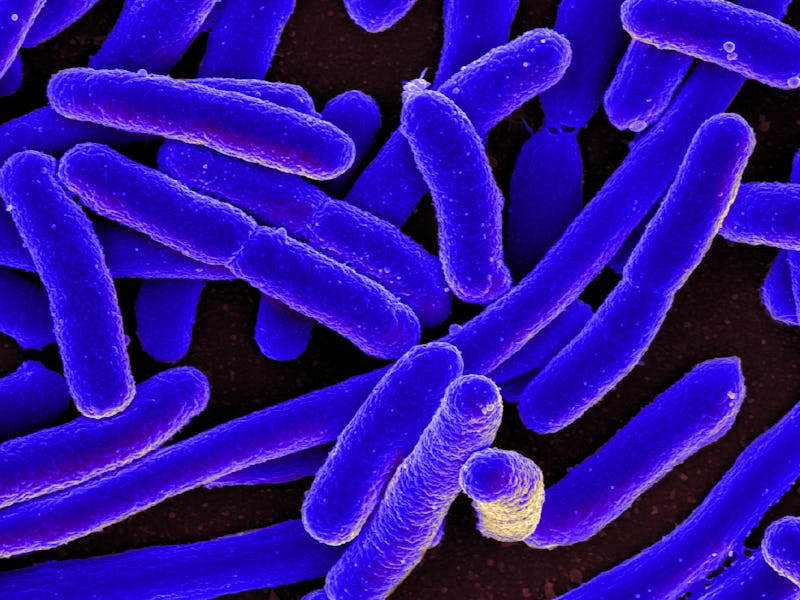
Take the widespread use of antibiotics in agriculture as an example: Drugs make animal husbandry, in particular, cheaper. Acknowledging and acting to minimize the dangers associated with dosing livestock, however, is expensive — albeit cheaper over the long term. In a paper recently published in The Lancet Infectious Diseases, Walsh and his team reported the discovery of an E. coli strain in China that eluded even Colistin, a last-resort antibiotic widely included in the country’s animal feed. Scarier still is the strain’s unprecedented ability to transfer resistance to its bacterial neighbors. Any animal — or human — unlucky enough to get infected by one of these super-resistant bugs has literally zero drug options for treatment.
This is frightening, which is presumably why the reaction was swift: The Chinese government has moved to remove the drug from its farms. The U.K.’s agricultural and veterinary sectors decided to put restrictions on Colistin use last week, even though resistant bacteria haven’t been found in Britain yet. “It’d be nice if other countries responded as quickly,” says Walsh, who knows that is asking quite a lot.
Farmers aren’t the only people with a lot at stake, he says. Hospitals and entire healthcare systems stand to lose business and public trust by admitting their practices are irresponsible. And it’s in the best interest of the companies that make the antibiotics themselves — located largely in China and Southeast Asia — that drug use carries on as usual. Like the bacteria themselves, the problem of antibiotic resistance could very well remain invisible until it’s not. Animals and people will get sick and there won’t be much we can do.
Asked point-blank whether he’s hopeful we’ll prevent the apocalypse, Walsh bluntly replies in the negative. But we might hold it off. The global antibiotic surveillance system he’s calling for, if it ever materializes (“I’m not really optimistic,” he says), won’t solve the problem but will at least buy us time. Even if scientists discovered a miracle drug — a “wondermycin,” as he calls it — it would take at least eight years of trials to get through the regulatory pipeline.
Organisms evolve, and so too must our strategies. In the little time we have left before the dawn of the post-antibiotic age, the entire paradigm of treating bacterial infections has to change. “We need to create an atmosphere of creative thinking and innovation,” says Walsh. “We need something completely novel.”